How Patients With Mental Illness and Hospitals in India are Coping with COVID-19
This story is reported as part of the India for Mental Health Fellowship launched in 2020 by Indiaspend in partnership with The Health Collective
By Riddhi Dastidar
New Delhi: For 14 years, Meenakshi Raman (name changed) had been taking her younger sister, 46-year-old Shruti (name changed), for treatment to the Institute of Human Behaviour and Allied Sciences (IHBAS) in New Delhi once a month. The sisters would spend the better part of the day there for Shruti’s treatment, occupational therapy and counselling for obsessive compulsive disorder (OCD) with bipolar affective disorder and traits of borderline personality disorder.
ALSO SEE: BORDERLINE PERSONALITY DISORDER
Their monthly routine was abruptly halted in March with the outbreak of COVID-19 and the subsequent lockdown. Shruti’s OCD symptoms and compulsive behaviours worsened due to her fear of infection. Without access to therapy and regular dosage of medicines–available for free at IHBAS’ outpatient department (OPD)–Shruti’s health deteriorated.

The doctors at IHBAS renewed Shruti’s prescription for medicines over WhatsApp in April so Meenakshi could buy them from the local chemist. Shruti’s monthly dose of Haloperidol, a prescription injection she received at IHBAS, proved challenging to procure. Meenakshi somehow managed to get the injection online from a private supplier and found a local doctor to visit their home in east Delhi to administer it to her sister. The family spent Rs 15,000 on the medicines and injections over five months between April and August.
Shruti is among thousands of Indians with chronic mental illness whose lives, and those of their caregivers, turned tumultuous after the pandemic hit. Pandemics are known to exacerbate mental health conditions, and India’s mental healthcare system failed to deliver during the COVID-19 crisis, as IndiaSpend reported in September.
As part of our Mental Health Fellowship in partnership with The Health Collective, IndiaSpend examined how patients, doctors and institutes coped. Over two months, we interviewed psychiatrists, superintendents and mental health professionals at 15 of 43 state-run mental health hospitals and institutions in the country, as well as independent experts, social workers and members of non-profit organisations working with stakeholders. The picture that emerged is one of an already overextended and under-resourced mental healthcare system unravelled by the COVID-19 crisis, leaving institutions and patients at sea and with little support from the central or state governments.
These 15 state-run mental health hospitals and institutions provide specialised tertiary care in 13 states–Andhra Pradesh (Visakhapatnam), Assam (Tezpur), Delhi, Gujarat (Ahmedabad and Bhuj), Himachal Pradesh (Shimla), Jammu, Karnataka (Bengaluru), Kerala (Kozhikode), Maharashtra (Thane and Nagpur), Meghalaya (Shillong), Nagaland (Kohima), Telangana (Hyderabad) and Tripura (Agartala).
They told IndiaSpend that while OPD patient numbers dropped drastically in the initial weeks of the lockdown, they found themselves under-staffed, overburdened and poorly-equipped to provide services between end-March and August. The fear that COVID-19 would spread affected operations and service delivery.
People living with chronic mental illnesses were unable to access state mental hospitals for care and were unable to procure and/or afford medication, we found. It was “weeks to months” before they were able to access hospitals, and many had relapsed or experienced psychosis. This was especially the case for patients who relied on hospitals across state borders due to restrictions on train services. As a result, many had to be admitted as in-patients, psychiatrists and medical superintendents at these hospitals said.
In addition, new patients were turned away from under-resourced hospitals for lack of beds, even as institutions were unable to discharge recovered patients so they could go home with their families. Homeless or wandering persons with mental illness brought to institutions by the police or under magistrates’ orders were both vulnerable to and a source of COVID-19 infections, and a challenge to treat when infected. Reintegrating such wandering persons–the process of locating and reuniting them with their caregivers–came to a near-complete halt, adding to the institutions’ workload.
IndiaSpend contacted the Minister for Health and Family Welfare, Harsh Vardhan, Minister of State for Health and Family Welfare, Ashwini Kumar Choubey and secretary, Department of Empowerment of Persons With Disabilities, and acting chief commissioner, Persons with Disabilities, Shakuntala Gamlin, to ask about the central government’s initiatives to minimise the adverse impact of COVID-19 on people living with psychiatric disabilities.
We have also contacted the health ministries in the 13 states. We will update this report when we receive a response.
Little understood, mostly ignored
“I started to panic before the PM could finish his speech [about a nationwide lockdown] on March 24,” said Anjlee Agarwal, founder of disability advocacy organisation Samarthyam who lives with muscular dystrophy and is a member of the central government’s premier policy think-tank, NITI Aayog. “The lockdown started [at a day’s notice] without planning. Disabled people accessing health infrastructure, especially people with mental illness, were the last ones to be thought about.”
Agarwal, who was instrumental in facilitating e-passes for caregivers of persons with disabilities during the lockdown, told IndiaSpend that it was mainly “benchmark disabilities”, where a person is certified as having at least 40% disability, that were considered in India’s disability response. Despite mental illness being recognised as a disability in the Rights of Persons with Disabilities Act 2016, getting this certification has proven a struggle, disabled peoples’ organisations told IndiaSpend.
Care for mental illness as a psychosocial disability is adjudicated by two ministries–the Ministry of Health and Family Welfare (MoHFW) and the Ministry of Social Justice and Empowerment (MoSJE)–whose functions overlap.
The MoHFW governs provision of services such as medication and treatment at primary health centres (PHCs) at the community level and specialised tertiary healthcare at state mental hospitals. The delivery of these services is the direct responsibility of state governments since health is a state subject. The MoSJE governs social security-related issues such as disability pension, reservations for employment and housing for homeless persons living with mental illness.
Reflecting this split, matters pertaining to mental health are regulated under the Mental Health Care Act of 2017 and the Rights of Persons with Disabilities Act of 2016.
Given that mental health involves both medical treatment and social welfare, there is an overlap between the two ministries but not enough intersectoral coordination, said Soumitra Pathare, director of the Centre for Mental Health Law and Policy (CMHLP), Pune. Instead, there is an overreliance on the idea of mental illness as a medical problem to be treated by a psychiatrist in a hospital, he said.
One in seven people or a total of 197.3 million people live with mental illness in India, according to the 2019 Global Burden of Disease Study, which analysed the prevalence and state-specific trends for different mental disorders in India from 1990 to 2017.
Nevertheless, mental illness is poorly understood. At least one survey of 3,556 respondents found that 62% used terms such as ‘crazy’, ‘mad’, ‘stupid’, ‘careless’ and ‘irresponsible’ to describe people with mental illness. From problematic reporting on suicide to the spectacle of the Sushant Singh Rajput case while an actual public health crisis for persons with mental illness was unfolding, we have a long way to go, Pathare said.
Only about one in 10 people with mental health disorders are thought to receive evidence-based treatments in India, the latest National Mental Health Survey (NMHS) found in 2016. It is estimated that 68-98% patients are able to access care for the first time at a district or tertiary state mental hospital, and not at a neighbourhood PHC.
This can partly be attributed to the lack of district-level presence of mental healthcare facilities, experts told IndiaSpend. The District Mental Health Programme (DMHP) was launched in 1996 under the National Mental Health Programme to decentralise treatment and provide mental healthcare integrated with general healthcare within the community itself i.e., at the district, block and PHC levels, under supervision of a district team.
When the pandemic broke out, the National Institute of Mental Health and Neurosciences (NIMHANS) in Bengaluru released COVID-19 guidelines for mental healthcare settings on behalf of the MoHFW on April 13. The guidelines propose management and community care of at-home patients with severe mental disorders through existing community outreach programmes, such as the DMHP.
When COVID-19 hit, the DMHP’s response largely involved ameliorating the distress caused due to the pandemic by prioritising psychosocial support to COVID-19 patients and quarantined persons. Dedicated helplines were set up to supplement the regular DMHP activities, mental health professionals and state nodal officers in Andhra Pradesh, Assam, Delhi, Gujarat, Kerala and Tripura told IndiaSpend. The response also focussed on ensuring continued supply of medicines and targeted psychosocial support to vulnerable populations such as in beggar homes, migrant worker shelters, and rural and tribal communities far from hospitals.
The DMHP, however, has a limited reach, NMHS said: “Despite 3 decades of implementing the NMHP, the proportion of districts covered by it ranged from 13.64% in Punjab to 100% in Kerala… Only 1/3rd of the surveyed states had more than 50% of the population covered by DMHP.”
Its implementation is inadequate even in the national capital, where the initiative is anchored by IHBAS. The DMHP team from IHBAS makes weekly visits to designated clinics in six of Delhi’s 11 districts. “Jahangirpuri and Chhattarpur have larger populations, so we visit twice a week,” said Pravin Yannawar, a psychiatric social worker at IHBAS. “Ideally, every district should have a community outreach programme.”
This lack of integrated mental healthcare and overreliance on tertiary state-level hospitals led to a crisis for these hospitals and their users in the months after the COVID-19 lockdown was imposed, IndiaSpend found.
“The COVID-19 crisis did not create new shortcomings,” said Pathare of CMHLP. “The crisis laid bare the existing shortcomings that have plagued the mental health system for years.”
Staff infected, hospital beds full
The COVID-19 crisis’ impact on mental health institutions instantly manifested in three aspects: COVID-19 infections among staff and patients; a decline in OPD footfalls; and stoppage in admissions of new mental health patients due to a lack of beds, IndiaSpend found.
Eight of the 15 hospitals IndiaSpend spoke to reported COVID-19 infections among hospital staff and patients, with infections among staff outnumbering those among patients.
Class 3 and 4 workers, i.e. clerks, ward attendants, nurses and cleaners were the ones to report the most COVID-19 infections. For instance, at the Regional Mental Hospital (RMH) in Thane, Maharashtra, nine staff had tested positive by June 19, the hospital’s medical superintendent, Sanjay Bodhade, told IndiaSpend. On August 11, seven female inpatients at RMH Thane, who had lived there for over 15 years, were reported to have tested positive for COVID-19, and were subsequently transferred to the civil hospital’s COVID-19 centre.
Many staff members commute from the suburbs of Mumbai where they live in crowded quarters in which social distancing is not possible, Bodhade said.
“There is also the economic imperative… many hospitals employ contractual employees who do not get paid leave and cannot afford to miss work,” Pratima Murthy, who heads the psychiatry department at NIMHANS, told IndiaSpend in August.
From March to August, 23 patients and 34 staff tested positive for COVID-19 at IHBAS Delhi, according to superintendent Deepak Kumar. Among the staff, most were attendants and nurses in contact with homeless persons admitted to the hospital or those working in the Emergency or COVID-19 isolation ward, he said. Many of them were asymptomatic, and the infection spread to colleagues, patients and families.
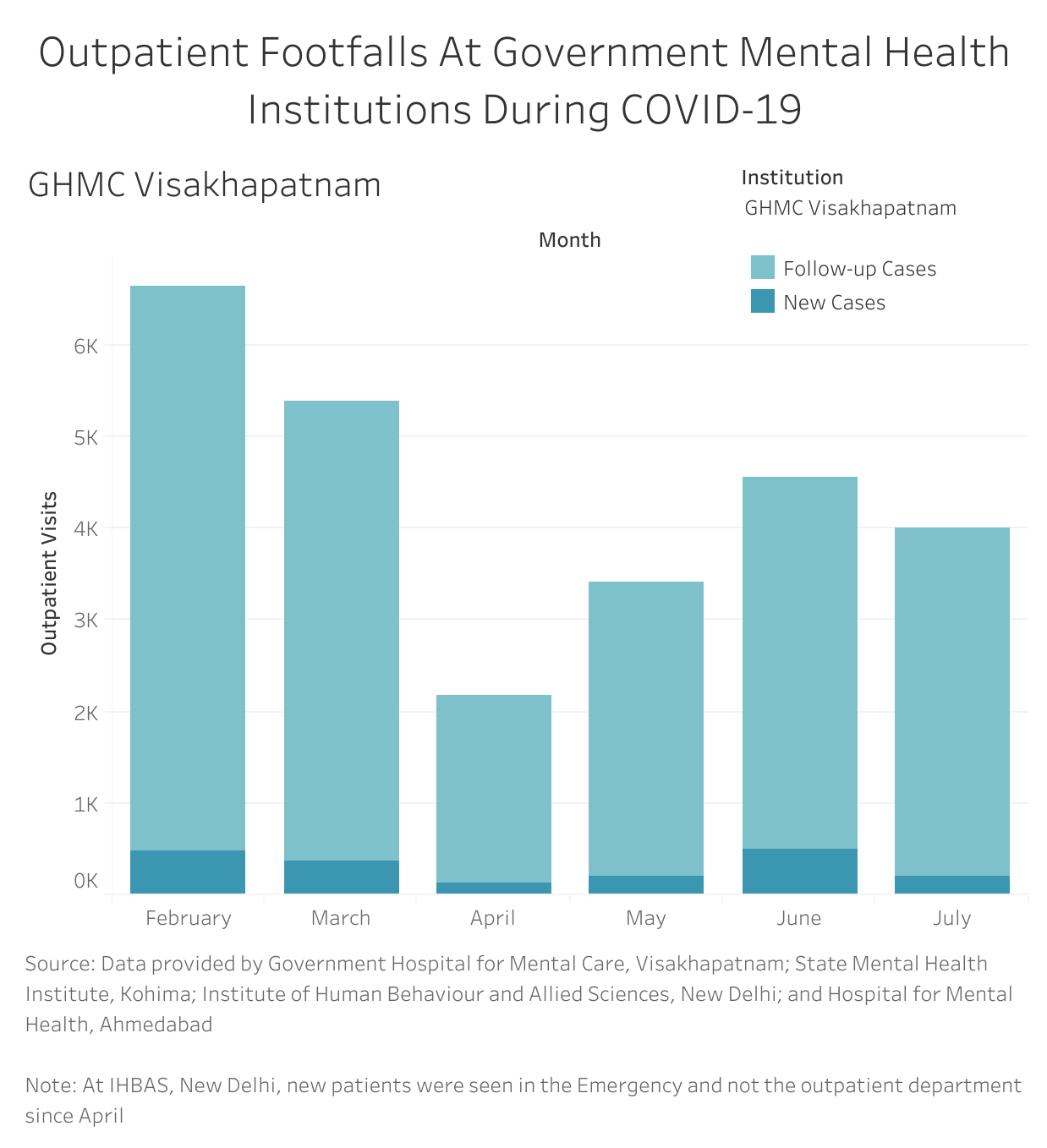
All 15 mental health hospitals and institutions that IndiaSpend spoke to reported a 20-50% drop in OPD footfalls due to the lockdown and stoppage of public transport between late-March and mid-August.
IHBAS reported nearly an 80% drop in OPD footfalls in April (5,401) when the 21-day lockdown was in place) compared to February (25,943), as per the institute’s records.
When lockdown restrictions started to ease in July, 16,924 patients went through IHBAS’ OPD. “We are trying to maintain as much social distance as possible but numbers are swelling at the OPD. Initially it was 600, then 800, today it was 1,060,” Kumar told IndiaSpend on August 8. Including caregivers, this comprised a 2,000-plus crowd with queues spilling from the IHBAS campus to the street outside.
While OPD footfalls dropped, there was a spike in emergency admissions for alcohol and opioid withdrawal, superintendents and officials at IHBAS, NIMHANS, Himachal Hospital of Mental Health and Rehabilitation (HHMHR) Shimla, Institute of Mental Health (IMH) in Hyderabad, Telangana and the Hospital for Mental Health (HMH) Bhuj in Gujarat, told IndiaSpend.
By late-July and early August, inpatient wards at most of the 15 mental health hospitals IndiaSpend spoke to were overcrowded or reaching full capacity, and new patients were being turned away. Mental health hospitals restricted inpatient admissions only to the “most severe cases” that could not be “managed at home”, and created isolation wards to quarantine and test new patients prior to admissions, superintendents and psychiatrists at 15 state mental hospitals told IndiaSpend.
At HHMHR Shimla, which has 50 psychiatric and 12 rehabilitation beds, wards were running full until late-July, Sanjay Pathak, senior medical superintendent, told IndiaSpend in an email. This is because reintegration–discharging inpatients to their families–had been rendered impossible and new patients could not be admitted because there were no unoccupied beds.
Beds were also full at the 40-bed HMH Bhuj; all 15 inpatients at Jammu’s Psychiatric Disease Hospital (PSD) were moved to a ward at the Government Medical College in late-July as PSD was converted into a COVID-care centre, doctors at the hospitals told IndiaSpend.
In the seven northeastern states, all the four state hospitals–Lokpriya Gopinath Bordoloi Regional Institute of Mental Health (LGBRIMH) in Tezpur, Assam; Modern Psychiatry Hospital (MPH) in Agartala, Tripura; Meghalaya Institute of Mental Health and Neurological Sciences (MIMHANS) in Shillong, Meghalaya; and State Mental Health Institute Kohima (SMHIK) in Nagaland–found themselves overburdened, psychiatrists, medical superintendents and DMHP officers told IndiaSpend.
The 50-bed MPH Tripura, the second-largest mental hospital in the northeast after LGBRIMH Tezpur, has been chock full. “There are about 250 inpatients at the hospital at any given time… five times the capacity,” Udayan Majumdar, state nodal officer for DMHP in Tripura, told IndiaSpend. “With just 50 beds, everything has to be compromised. We need more infrastructure.”
At MIMHANS in Shillong, 130 of 150 beds were occupied in late-July with 16 beds diverted for a COVID-19 quarantine ward, said S Lyngwa, the psychiatrist at the hospital. MIMHANS serves people not just from Meghalaya but also from Nagaland and Assam.

COVID-19 crushed overburdened staff
Lyngwa has been the sole psychiatrist at MIMHANS since 2019 when the other psychiatrist was moved to the Civil Hospital, according to superintendent Badira Mawlong. MIMHANS is trying to find another psychiatrist “but there are very few in Meghalaya”, Mawlong said.
“Most patients here require close observation and the burden is very heavy,” Lyngwa told IndiaSpend, adding that she makes do with “two medical officers who have some idea about psychiatry and 30 nursing staff”.
The shortage of psychiatrists and caregivers is not unique to MIMHANS. Delhi’s IHBAS is “running with 23% of sanctioned posts”, according to its head of psychiatric social work, Jahanara Gajendragad. Eleven of 15 state-run mental health hospitals contacted by IndiaSpend reported that they have been facing a staff shortage since March.
The lack is reflected in the poor ratio of mental health professionals to the population in the country. Per 100,000 people, India has approximately 0.29 psychiatrists, 0.07 clinical psychologists, 0.06 social workers and 0.80 nurses, according to a 2017 profile of India by the World Health Organization.
Staff were further diverted for COVID-19 duties, had to undergo mandatory quarantine for 10-14 days thereafter, and many others were unable to commute to work because public transport was shut during lockdown 1.0, superintendents and medical officers told IndiaSpend. The burden of care on the available staff during the early months of the COVID-19 outbreak has been tremendous, they said.
“Most staff are under severe pressure,” said V.V. Asha, superintendent at the Government Mental Health Centre (GHMC) in Kozhikode, Kerala, where almost all sanctioned posts had been filled but staff had been diverted to COVID-19 care centres.
HHMHR Shimla functioned with 50% strength during the complete lockdown, said Pathak. At SMHIK Nagaland, one of three doctors was engaged in COVID-19 duty initially and class-3 staff until August, medical superintendent T Wabang told IndiaSpend.
Teleconsultation, longer-term prescriptions
Mental health hospitals and institutions adapted to the crisis by setting up teleconsultation for patients and caregivers unable to commute due to lack of public transport.
At NIMHANS, a continuum of care was set up during the lockdown, Murthy said: since regular patients’ contact numbers were available, NIMHANS connected them to the dispensaries of their local civic body, the Bruhat Bengaluru Mahanagara Palike, where medicines were made available. “Training doctors at dispensaries [so they could interact with mental health patients] was simple,” Murthy said. “Given the shortage of psychiatrists in India, all cadres of medical staff ought to have some idea of mental illness. It is crucial to make this training and medication available at local community health centres across the country even beyond COVID.” Training of medical staff about basic mental health is a crucial aspect of the DMHP programme.
Additionally, some doctors wrote out slightly longer-term prescriptions, particularly for persons with chronic and severe psychiatric conditions. For instance, as OPD footfalls dropped from an average of 400 per day to 80 in April, doctors at Government Hospital for Mental Care (GHMC) Visakhapatnam in Andhra Pradesh started writing out prescriptions–on WhatsApp–for two months instead of for 15 days to one month, according to medical superintendent Radha Rani.
Longer prescriptions carry potential pitfalls and so the custom has not been uniformly practiced. “At IMH Hyderabad, medication is not prescribed for more than one month because we do not know how it might be used,” medical superintendent Uma Shankar explained.
Discharge, reintegration slowed; rehabilitation suspended
Seven of 15 hospitals told IndiaSpend that patient discharges slowed down and reintegration of wandering or homeless patients grinded to a halt.
“Families of long-term inpatients were unable to visit them in the hospital or get them discharged,” said Ajay Chauhan, medical superintendent of Hospital for Mental Health (HMH) Ahmedabad. “This was partly due to the lockdown restrictions and partly due to fear of [contracting the] infection. Patients are upset because they have not met their families for weeks.”
Occupational therapy and vocational therapy–essential for people with mental illness to develop social skills and become economically independent–facilitate their reintegration into community living. These therapies and rehabilitation services were halted due to COVID-19 caution. “The social and physical distancing is the opposite of this [socialising during therapy],” said Murthy of NIMHANS. “We’ve lost five months.” These services are restarting at varying speeds and scales in different states, our sources at the various institutions told us.
Occupational therapy remained halted in some facilities until mid-October.
Reintegrations had stopped for patients whose families were untraceable, typically patients found wandering or homeless. At GMHC Kozhikode, a ‘discharge adalat’ (court) traces the relatives of people who have been admitted to hospital as wandering or homeless persons. There are 60-90 such inpatients at the hospital at any given time, said superintendent Asha. “Since COVID-19, even if willing relatives are located, they have not been able to travel to take the recovered patients home.”
By mid-October, reintegrations had resumed at IHBAS in Delhi, NIMHANS in Bengaluru, HMHM in Ahmedabad, MIMHANS in Shillong and at a few more places.
The activities of the visitors’ committee, which oversees reintegration at the Regional Mental Hospital, Thane, had been at a standstill since April, said Bodhade. This is partly why the 1,850-bed hospital remained overcrowded until late-July.
“Patients are restless after having had to spend three months in the hospital,” said Madhuri Thorat, medical superintendent at the Regional Mental Hospital at Nagpur, Maharashtra. “We were under the impression that the coronavirus restrictions would taper off in one or two months,” she told IndiaSpend in July.
The discharge committee was operating in October, Thorat said when we followed up with her. “Almost all patients with known caregivers have been discharged; transport restrictions have compelled them to use ambulances. While the majority of homeless patients are still at the hospital, two such persons were reintegrated to Assam and Bihar. RMH Nagpur is not facing the crisis of overcrowding that it was in August.”
The Mental Health Care Act 2017 requires the government to provide “less restrictive community based establishments including half-way homes, group homes and the like for persons who no longer require treatment” in restrictive mental health establishments.
Such rehabilitation facilities are either missing or inadequate in India’s landscape of mental healthcare services, counsellors and stakeholders told IndiaSpend. The central and state governments have yet to comply with a 2017 SC direction to set up or expand such half-way homes. As of 2020, the states have provided a road-map towards implementation.
Bottom-up strategies work
Mental health professionals told IndiaSpend that the effective implementation of DMHP is key to resolving many critical issues that mental healthcare delivery faces in India.
Kerala, the only state with 100% DMHP coverage in all 14 districts per the NMHS, seems to be a case in point. All the districts have a psychiatry unit either at the general hospital or at the district hospital and at a few block hospitals as well.
The DMHP in the state functions as envisioned: a bottom-up initiative in which accredited social health activists (ASHAs) keep track of mental health incidences in their respective communities. They report these to doctors at PHCs, family health centres (FHC) or community health centres (CHC). The doctors in turn refer patients to the monthly DMHP clinics at the local PHC or at one of three tertiary state-level mental hospitals.
“On average, 40,000 patients visit DMHP clinics [at PHC/FHC/CHC] each month across the state,” Kiran P.S, state nodal officer for DMHP, told IndiaSpend.
This local access to treatment facilities has eased the pressure on tertiary care units, including state-run mental health hospitals. “Even before COVID-19, most patients did not come to the OPD at the [GHMC Kozhikode] hospital because they are being taken care of in respective [DMHP] centres,” Asha said.
This is the reason patients were able to get medicines at their nearest PHC across 14 districts even during the complete lockdown from March 24 to May 17 when DMHP clinics and the daycare centres under the state’s mental health-for-all programme, Sampoorna Manasikarogyam, remained shut. “The number of [patients with] relapses has therefore not been high [during the lockdown],” Kiran said.
That this bottom-up approach is effective becomes apparent in the OPD footfalls at GMHC Kozhikode, one of the three tertiary care hospitals in the state. There were 200 OPD patients on an average per day before COVID-19, according to Asha. “Now [in late-August], we have about 150 people per day.”
Lessons from COVID-19 crisis
The COVID-19 pandemic has made a strong case for integrated mental healthcare, Pathare of CMHLP said. “We need two things: First, a mental healthcare system modelled on reproductive and child health–with services starting at the village level and going up to the tertiary hospitals,” he said. “Second, we need better intersectoral coordination between mental health and social welfare departments of the government.”
More than anything, he said, India needs “programmes that support people to continue living in the community”. The Banyan’s Home Again programme, which provides health and social care together, is an excellent example, he said.
Shifting care away from institutions to communities is what the UN Policy Brief on COVID-19 and Mental Health also recommended.
Bincy P Chacko, who leads aftercare services at The Banyan’s Kerala chapter, told IndiaSpend that the country must bolster outpatient services and have daycare centres where persons living with mental illness who need acute care can be cared for during the daytime instead of being institutionalised. IndiaSpend had earlier reported on this long-term rehabilitation strategy in September 2018.
Indeed, a task force proposed a national strategy in the National Mental Health Report for inclusive and community-based living for persons with mental health issues in 2019. It conducted a field-study across the country’s 43 state-run mental hospitals and found that 6.1% of inpatients stayed in mental hospitals for over five years.
The report outlined an action plan towards de-institutionalisation, including an expansive community care system allied with the social care sector to prevent re-entry into homelessness or long-term institutionalisation, specific investments for defined pathways from hospitals towards person-centered community living, support towards key social entitlements such as disability allowance and voting rights, and decentralising bed capacities from tertiary to district and block-level hospitals.
The recommendations have remained on paper, particularly as healthcare focus has shifted to COVID-19 in 2020. Nevertheless, COVID-19 has brought into the spotlight the dangers of a mental healthcare system primarily dependent on overburdened tertiary state mental hospitals. Whether this will lead to scaling up of the DMHPs and the national strategy’s action plan remains to be seen.
(Riddhi Dastidar is a writer and researcher in Delhi. They hold an MA in Gender Studies from Ambedkar University, Delhi, where their research focused on embodiment and chronic psychiatric disability in women and queer persons. Riddhi lives with OCD and their work focuses on disability justice, gender and culture. Editing by Marisha Karwa/ Indiaspend.)




